Precision Medicine Applications
This isn't theoretical anymore - the subphenotype approach is already
informing medication choices in real clinics. Doctors are starting to
select treatments based on your metabolic profile rather than just
throwing darts at the diabetes medication board and hoping something
sticks.
Personalized Medication Selection
SGLT2 Inhibitors:
Work best for certain insulin-resistant subphenotypes, especially
those with liver involvement
GLP-1 Receptor Agonists:
Most effective when incretin pathways are intact - useless if your
problem is elsewhere
Insulin Therapy:
Requirements vary dramatically based on residual beta-cell
function
Metformin:
Works great for liver insulin resistance, less helpful for muscle
resistance
Lifestyle Intervention Targeting
Here's something that'll blow your mind - research shows that exercise
effectiveness for glucose control varies dramatically between
individuals. Some people can train like Olympic athletes and barely
budge their blood sugar, while others see massive improvements with
moderate activity. It's all about matching the intervention to your
metabolic subphenotype.
Subphenotype-Specific Exercise Recommendations
-
Muscle insulin resistance: Focus on resistance
training and muscle-building activities
-
Beta-cell dysfunction: Emphasize beta-cell
preservation through weight management
-
Incretin defects: Consider meal timing and
incretin-boosting activities
-
Hepatic insulin resistance: Target liver fat
reduction with specific exercise protocols
Discover Your Personalized Mediterranean Diet
Since different metabolic subphenotypes respond differently to
diets, get a customized Mediterranean approach that works with
YOUR unique physiology - not against it.
Heart-healthy fats
Anti-inflammatory foods
Metabolic optimization
Get Your Custom Mediterranean Plan →
The Future of Glucose Management
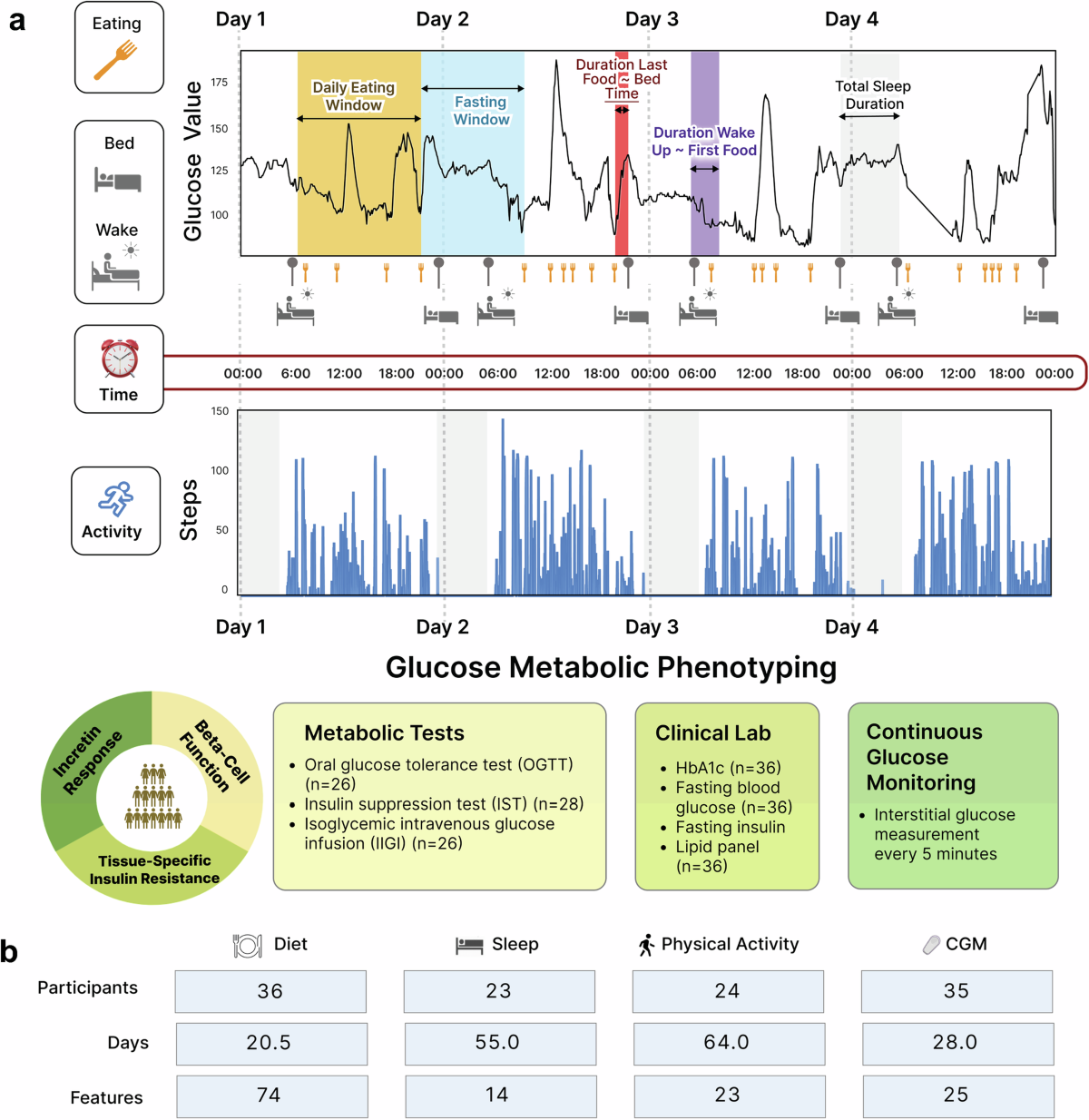
The ability to identify metabolic subphenotypes using CGM data
represents a paradigm shift from reactive to proactive diabetes
management. Instead of waiting for diabetes to develop and then trying
to manage it, we can now identify high-risk individuals and their
specific metabolic vulnerabilities years in advance.
Continuous Glucose Monitoring as Diagnostic Tool
Your CGM isn't just tracking your current blood sugar - it's providing
a window into your metabolic future. The patterns it reveals can
predict diabetes risk and guide prevention strategies years before
traditional tests would catch anything. It's like having a metabolic
crystal ball strapped to your arm.
Imagine getting a comprehensive metabolic report that says: "Based on
your glucose patterns, you have a 78% chance of developing muscle
insulin resistance within 5 years. Here's your personalized prevention
plan." That's not science fiction - it's the logical next step of this
research.
Clinical Translation Challenges
Of course, it's not all smooth sailing. Moving from research labs to
everyday medical practice has its challenges, and we're still working
through some significant hurdles that need to be addressed before this
becomes standard care.
Current Implementation Barriers
-
Standardization: Different studies use varying
criteria for subphenotype definitions
-
Cost-effectiveness: Determining when sophisticated
testing is justified
-
Training: Educating healthcare providers about
precision medicine approaches
-
Technology access: Ensuring CGM and machine
learning tools are widely available
The good news? These are solvable problems. The technology exists, the
science is solid, and the clinical benefits are clear. It's just a
matter of scaling up and standardizing the approach. Given how rapidly
digital health technology is advancing, I'd bet we'll see widespread
adoption within the next decade.
Implications for You
So what does all this mean for your actual health? Your personal glucose
patterns reflect your unique metabolic subphenotype, which explains why
you might experience different responses to the same meal as your
friend, why certain medications work better for you, and why your
optimal diabetes management strategy should be tailored to your specific
physiology.
Biomarker-Guided Treatment
The future of diabetes care will likely involve biomarker-guided
treatment selection, where your metabolic subphenotype determines your
therapeutic approach from the outset rather than the current
trial-and-error method. This personalized approach promises more
effective treatments with fewer side effects.
Custom Ketogenic Diet for YOUR Metabolic Type
Since we know that different metabolic subphenotypes respond
differently to dietary interventions, why not get a keto plan
designed specifically for your body's unique needs?
Personalized macros
Metabolic optimization
Custom meal plans
Glucose-friendly recipes
Create My Custom Keto Plan →
Understanding your metabolic subphenotype empowers you to make informed
decisions about lifestyle interventions, medication choices, and
monitoring strategies. Rather than following generic recommendations,
you can pursue targeted approaches that match your individual
physiology, potentially achieving better outcomes with less effort and
fewer side effects.
The End of One-Size-Fits-All Medicine
The discovery of metabolic subphenotypes represents the end of generic
diabetes treatment protocols. Your blood sugar behaves differently than
your friend's because you have different underlying metabolic phenotypes
that require different therapeutic approaches. This isn't just a minor
refinement of existing care - it's a fundamental shift toward precision
medicine that recognizes the biological reality of metabolic diversity.
The ability to predict these subphenotypes using CGM data with 95%
accuracy means that personalized diabetes medicine is not a distant
future concept but an immediate possibility. As this technology becomes
more accessible, we can expect a revolution in how diabetes prevention
and treatment are approached, moving from reactive management to
proactive, precision-guided care tailored to your unique metabolic
profile.
This research fundamentally challenges the traditional view of diabetes
as a single disease entity and instead reveals it as a collection of
distinct metabolic disorders that require personalized approaches. The
future of diabetes care lies in recognizing and treating these
individual differences rather than applying blanket protocols to
everyone. And honestly? It's about time.
Take Control of Your Metabolic Health
Ready to discover your unique metabolic profile? Start by
understanding your current glucose patterns and exploring personalized
approaches to blood sugar management.
Explore Blood Sugar Management Tools
Frequently Asked Questions
How can I find out my metabolic subphenotype?
Currently, metabolic subphenotyping requires specialized testing
that's mainly available in research settings. However, continuous
glucose monitoring combined with an oral glucose tolerance test
can provide valuable insights. Talk to your doctor about CGM
options and whether subphenotype testing might be available in
your area.
Will insurance cover metabolic subphenotype testing?
Insurance coverage for subphenotype testing varies and is still
evolving as the technology moves from research to clinical
practice. Some components like CGM may be covered if you have
diabetes, but comprehensive metabolic profiling may not be covered
yet. Check with your insurance provider about coverage for
advanced glucose monitoring and metabolic testing.
Can my metabolic subphenotype change over time?
Yes, your metabolic subphenotype can shift over time due to
factors like aging, weight changes, lifestyle modifications, and
disease progression. This is why periodic reassessment may be
valuable, especially if your response to treatments changes or
your health status evolves.
Are there any at-home tests available now?
While full metabolic subphenotyping isn't available at-home yet,
you can use continuous glucose monitors (available
over-the-counter) to track your glucose patterns. Some companies
are developing at-home metabolic testing kits, but these aren't
yet validated for clinical use. The technology is advancing
rapidly, so expect more options in the coming years.
How accurate are these predictions compared to traditional tests?
The machine learning algorithms show remarkable accuracy - up to
95% for predicting muscle insulin resistance and 88-89% for other
subphenotypes. This often exceeds the accuracy of traditional
single-point blood tests and provides more comprehensive
information about your metabolic function.
What should I do if my current treatment isn't working?
If your current diabetes treatment isn't working well, discuss
metabolic subphenotyping with your healthcare provider. Even
without formal testing, understanding the different subphenotypes
can help guide treatment decisions. Consider tracking your glucose
patterns with a CGM and discussing whether your medications match
your likely metabolic profile.